can you confirm the following First:
- Yes, I saw the whole video above and loved it!
- Yes, I’m a coach, expert, consultant, agency owner, course creator or I want to be one!
- Yes, I’m happy to invest in my success and understand that y’all guarantee success!
-
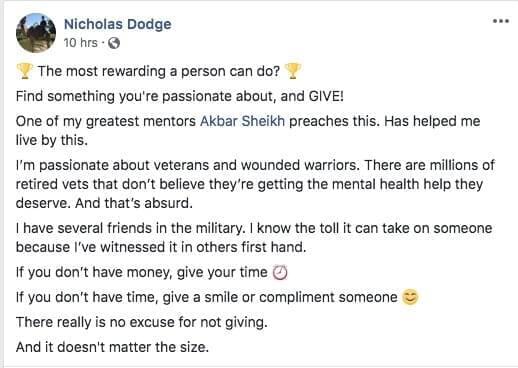
Yes, I want to MAKE MORE, so I can GIVE MORE!
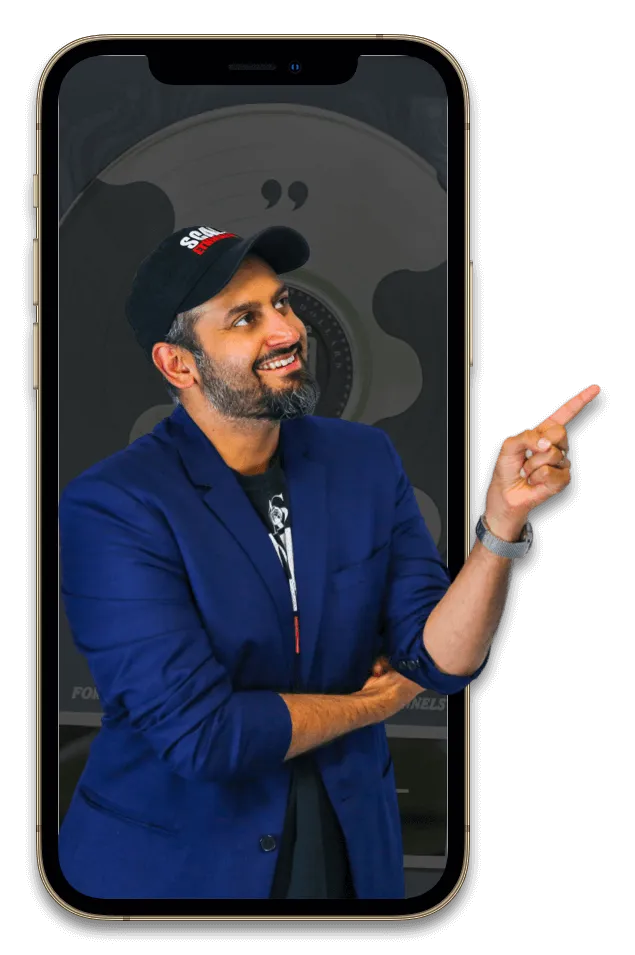
My Journey From homeless To The #1 Business Coach for Entrepreneurs Who want to Make More Give More
Akbar Sheikh
Years ago, I was living in an electrical closet with no windows, showers, or hot water. I was in a marriage from hell, had debilitating anxiety, and terrible addictions that held me back.
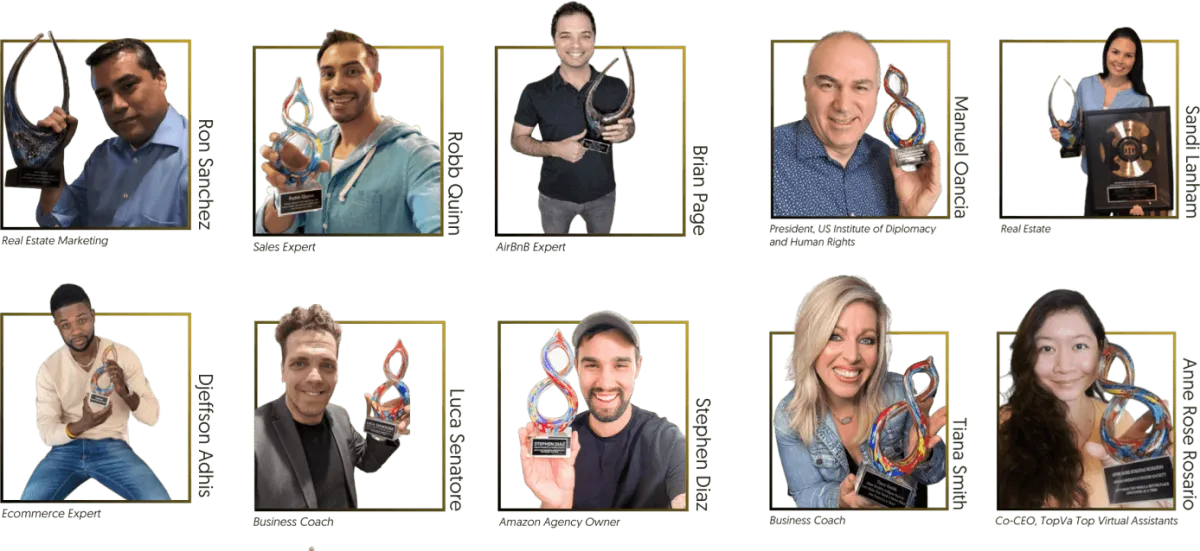
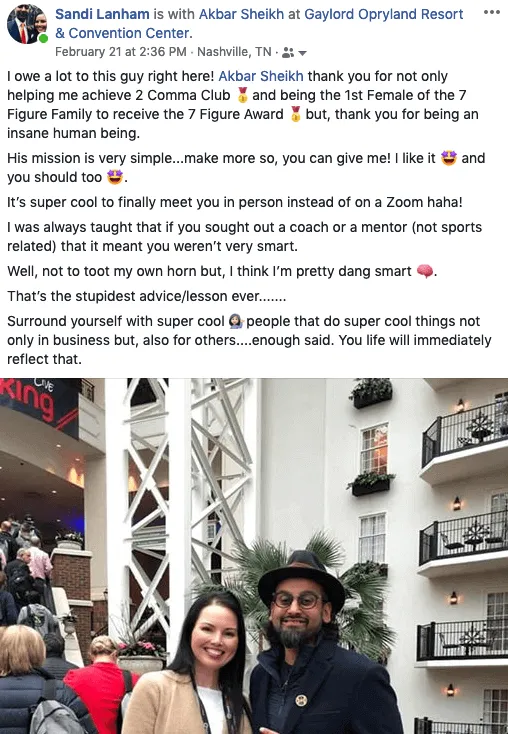
Fast forward to today, my team and I have handed out over 65 trophies to entrepreneurs that hit 6, 7, and even 8 figures.
Along the way, I lost 50lbs, got over my crippling anxiety disorder, and am enjoying a wonderful marriage with 3 crazy kids all the while doing philanthropic work around the world!
Our mission is very clear: We want to help YOU make more, so you can give more to your families, communities, and favorite charities, hence making the world a better place!
We have spoken around the world including TEDx Stage.. became a International #1 best selling author, and most importantly have build countless water wells, given the gift of vision to blind people, and sponsoring orphans around the world..


Akbar Sheikh
My journey from homeless to world-renowned coach

Years ago, I was living out of an electrical closet without hot water, was in a marriage from hell, had debilitating anxiety, and bad habits that held me back.
Fast forward to today and my team and I have helped countless entrepreneurs hit 6, 7, and even 8 figures.
Along the way, I lost 50lbs, got over my crippling anxiety disorder, and am enjoying a wonderful marriage with 2 crazy kids all while doing the work and living the life I love.
Our mission is very clear: We want to help YOU make more, so you can give more to your family, favorite communities, and charities, hence making the world a better place!

IT'S ALL ABOUT MAKING MORE
TO GIVE MORE

We don’t teach the Hustle culture, we teach a giving culture.
It's all about Making More to Give More.. Both we and our students are big supporters of building water wells, sponsoring orphans, and giving the gift of vision to blind children.
A portion of every sale goes towards making the world a better place.
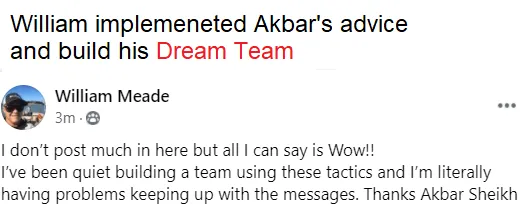
Experience some of our students' Success

When we help our clients hit 6-7-8 figures, we give them an amazing trophy...
(Can't Wait To Give You Yours)


Video TEstimonials Section
Tell me, akbar... Do You Have more amazing Testimonials?

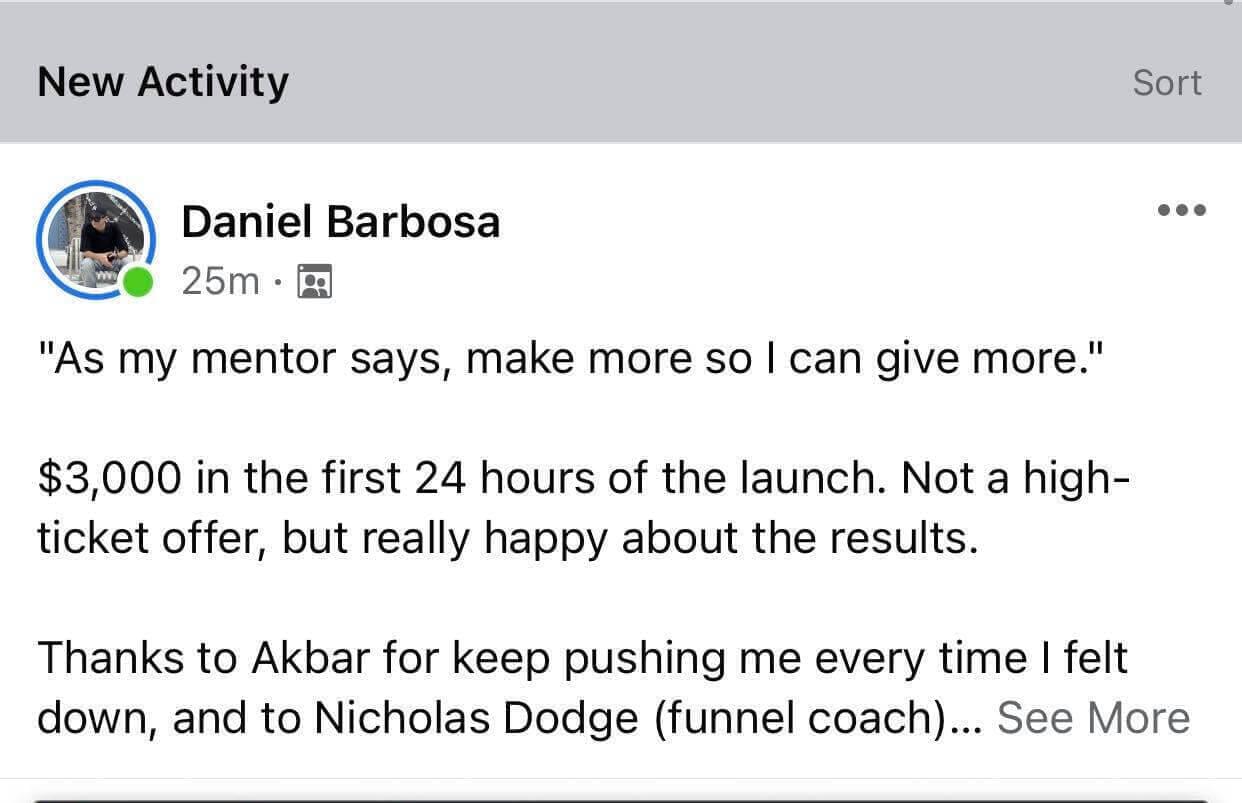
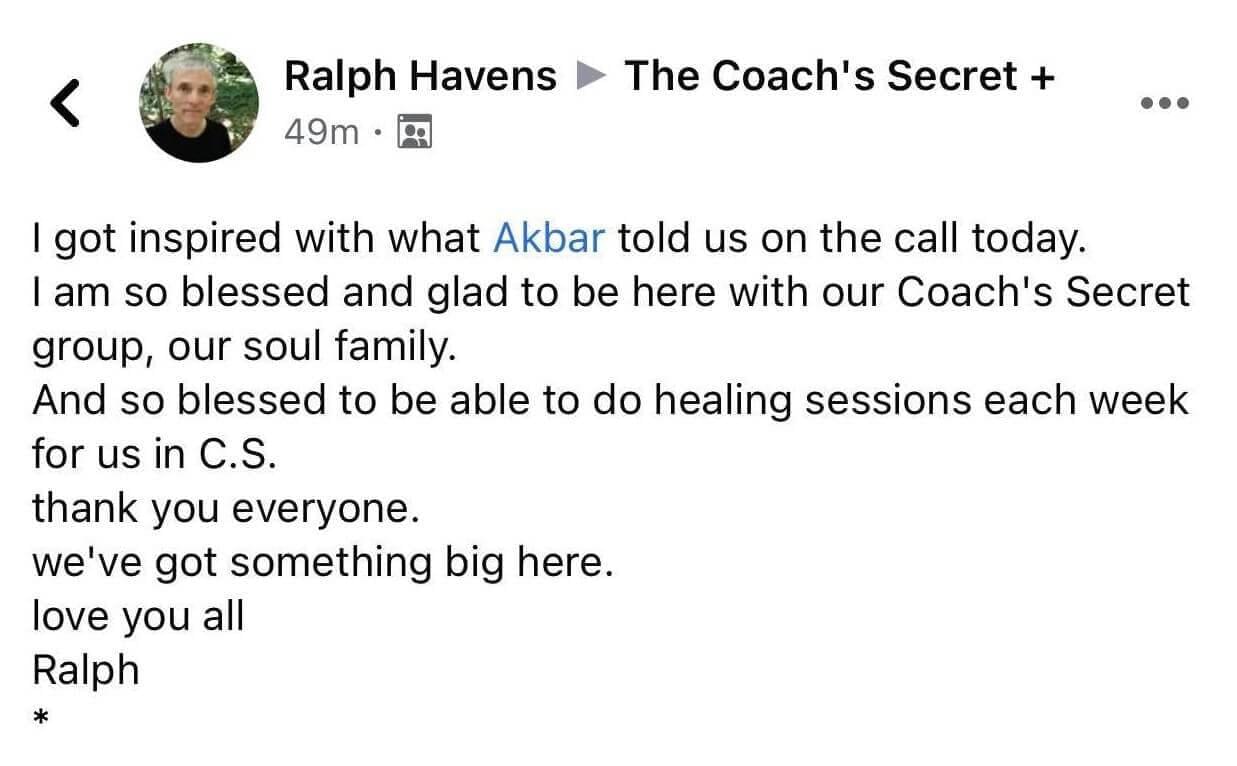
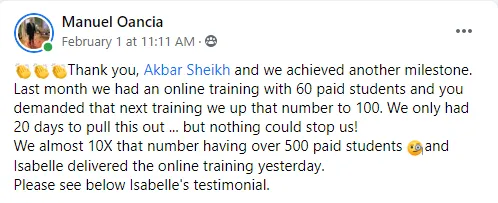
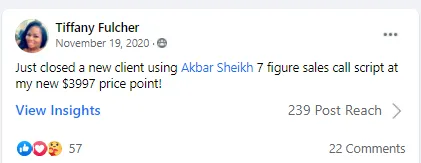
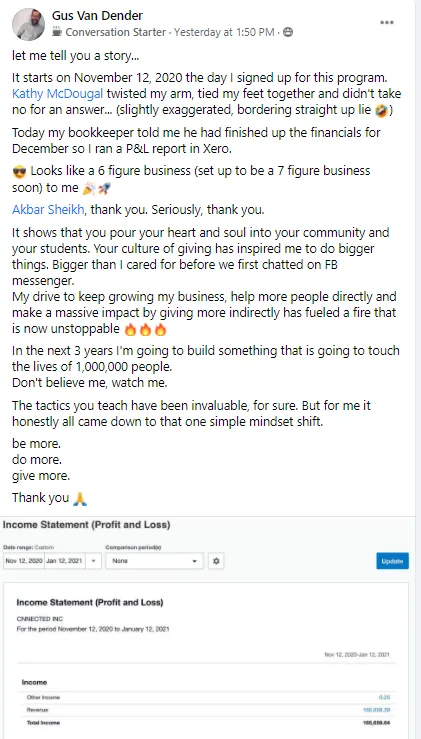
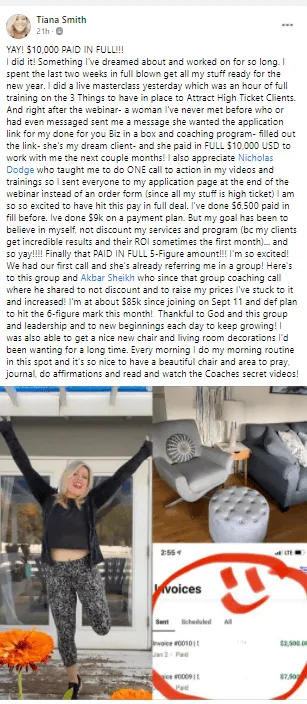

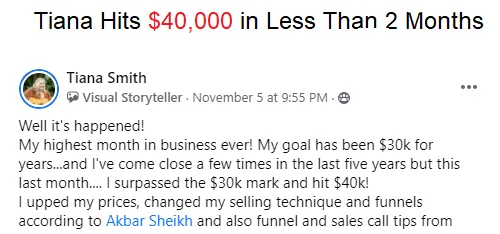
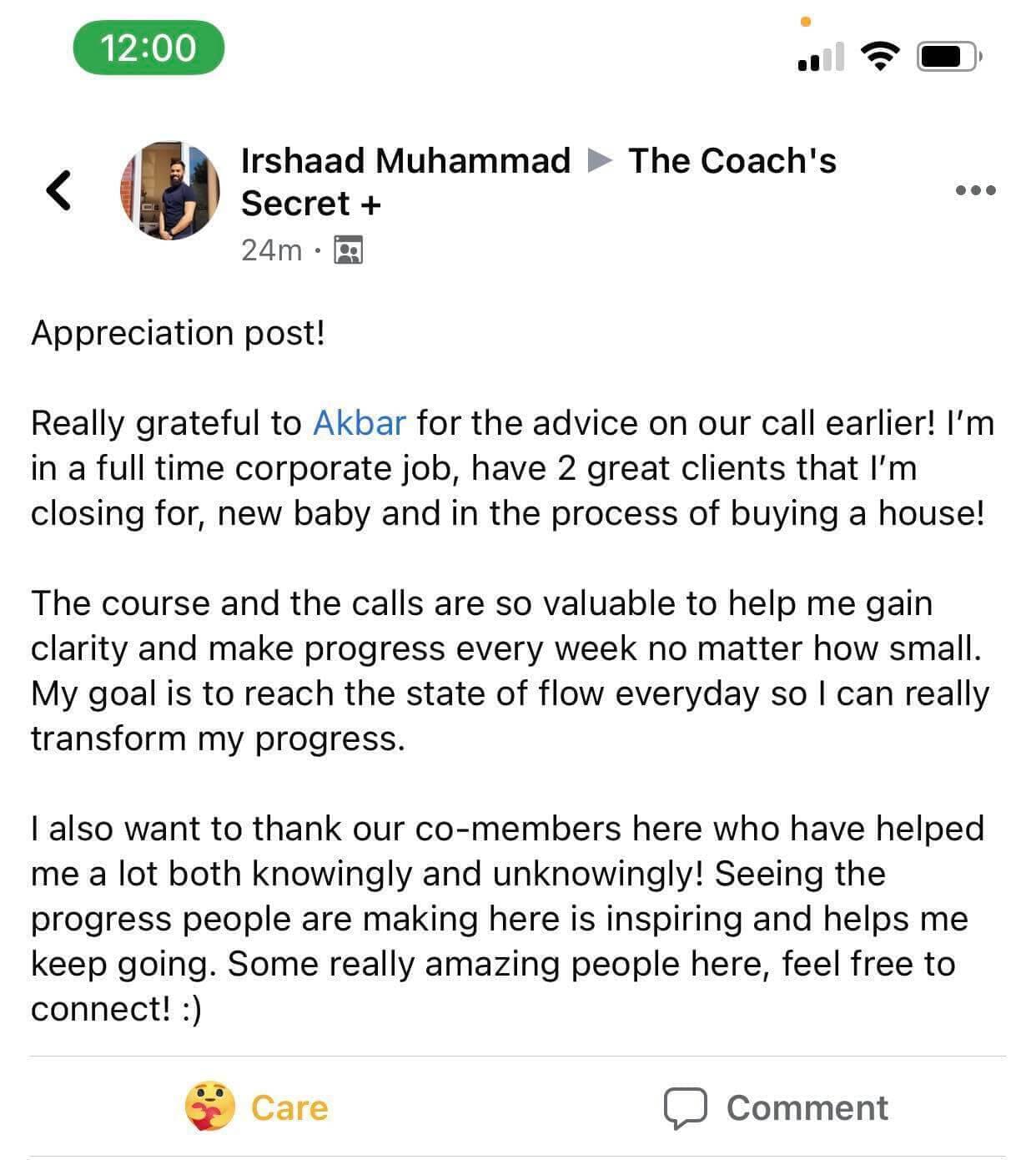
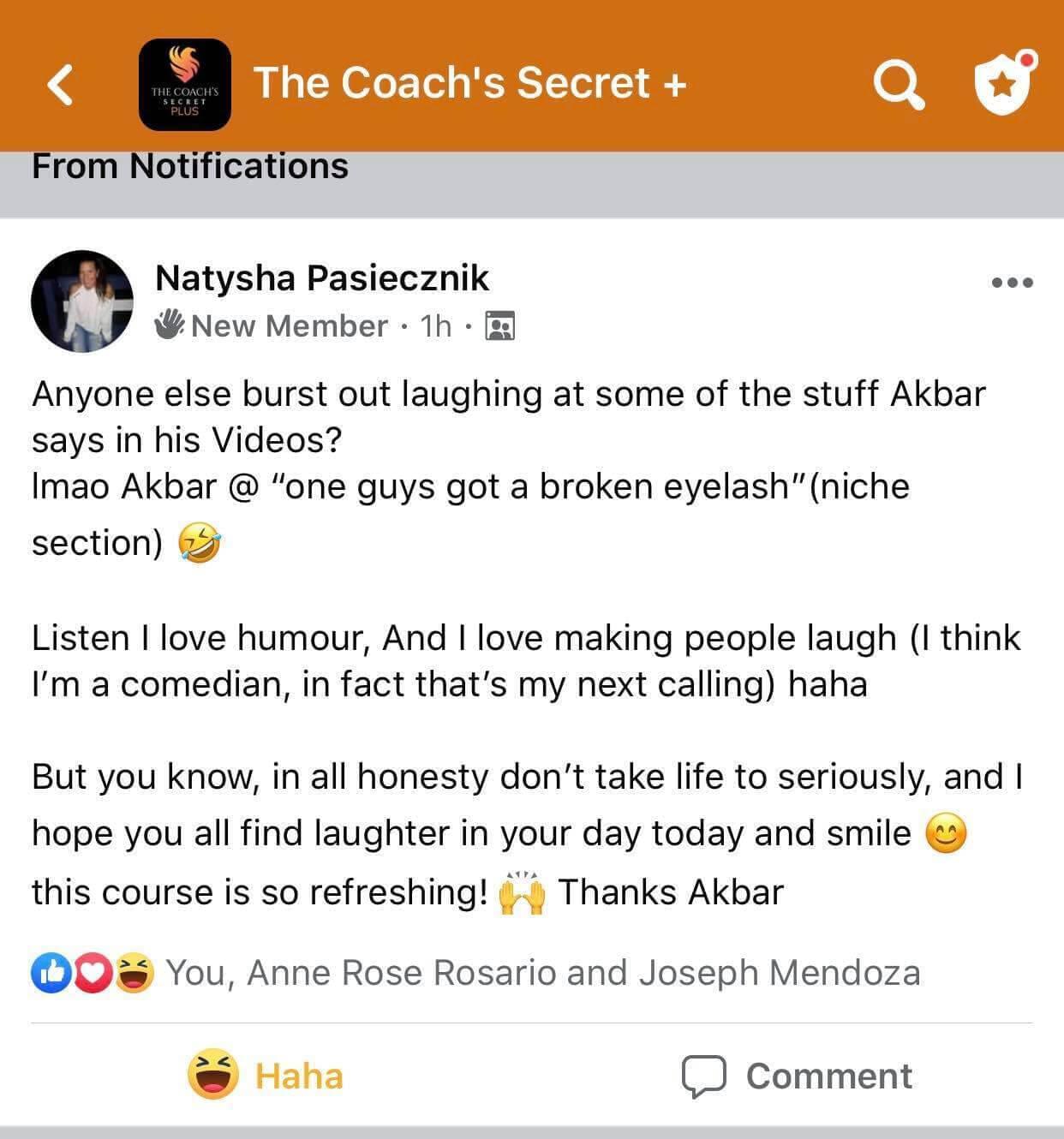


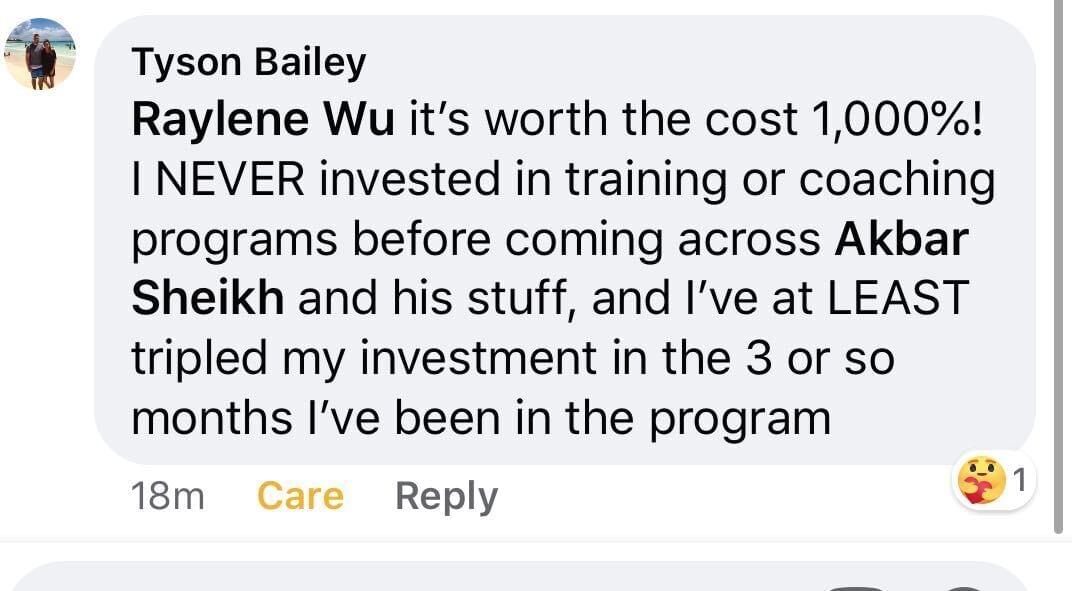
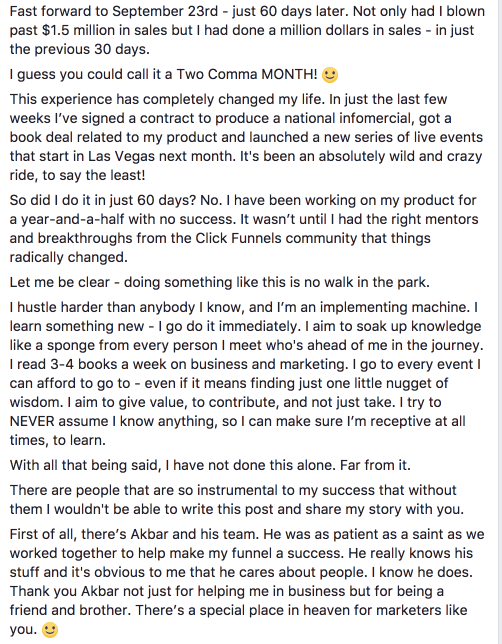

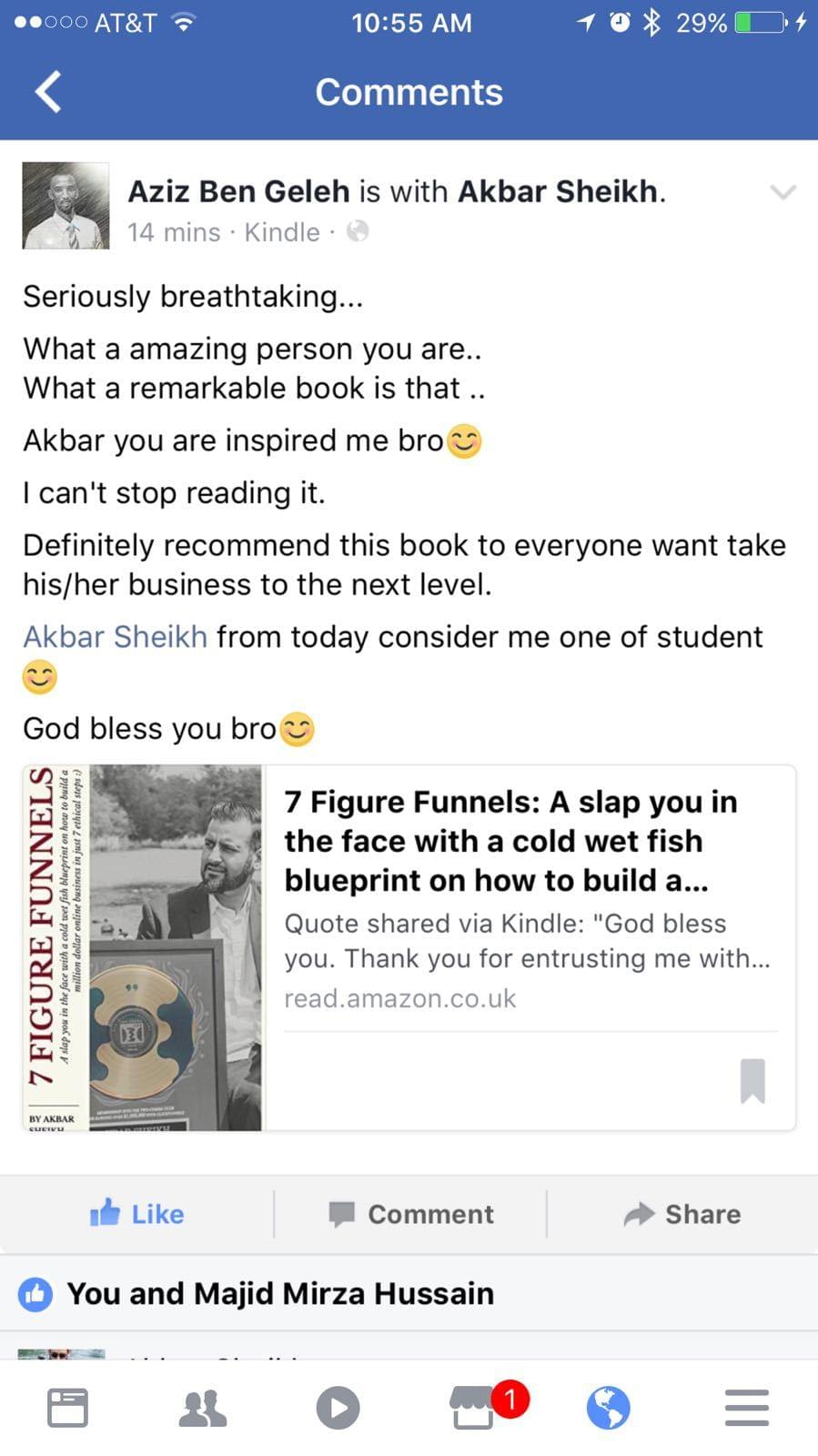
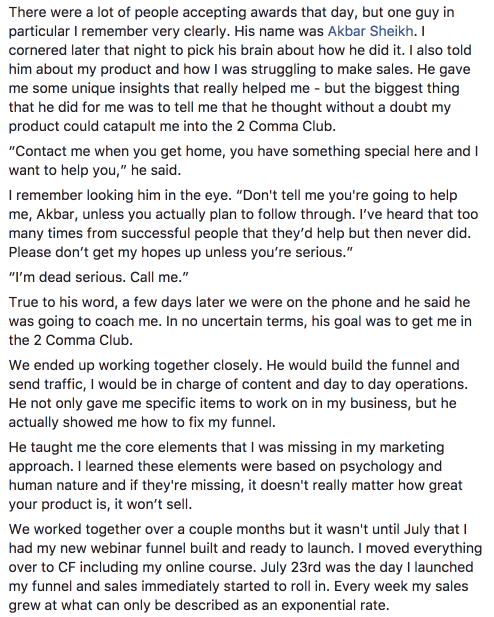
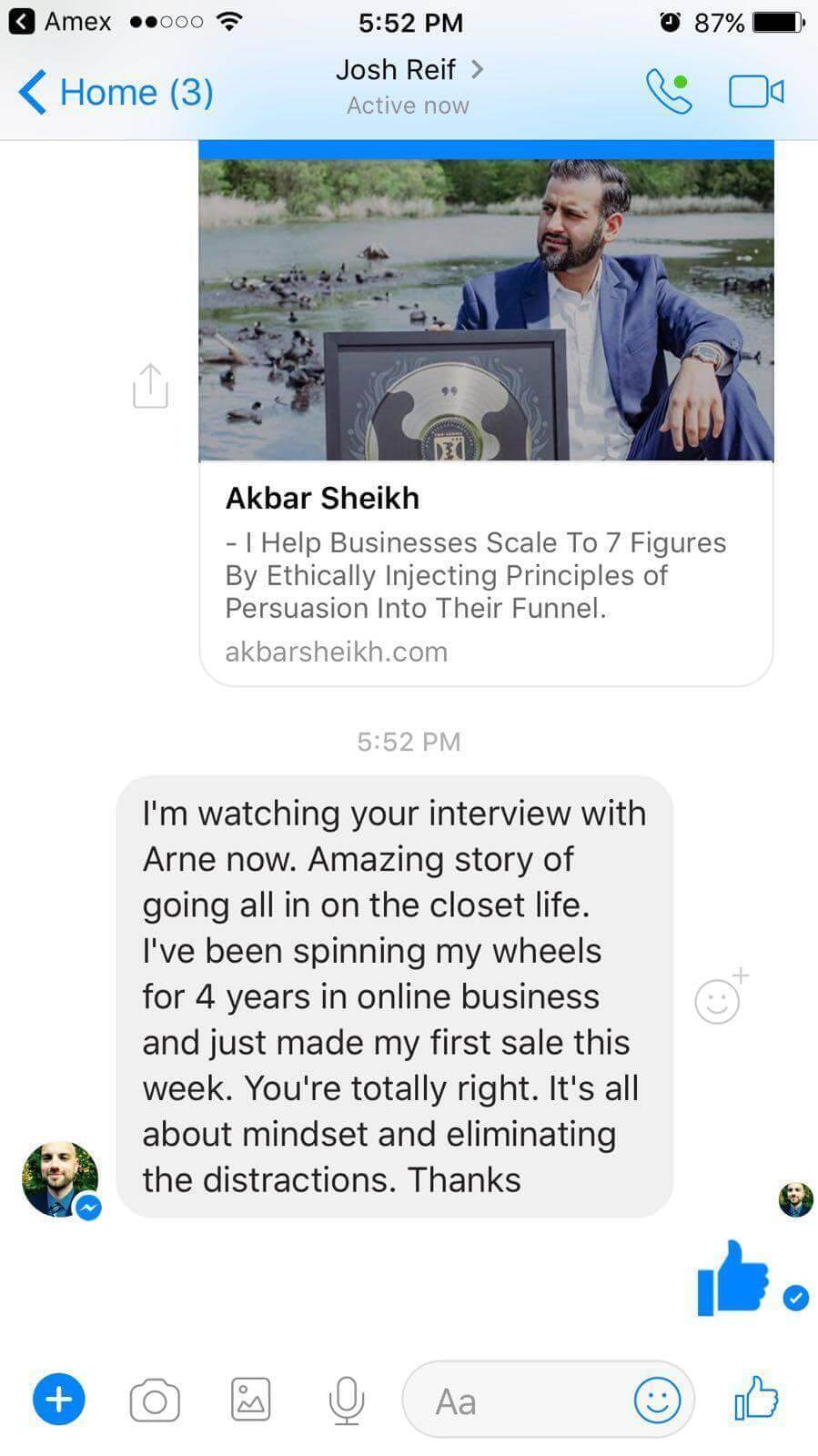
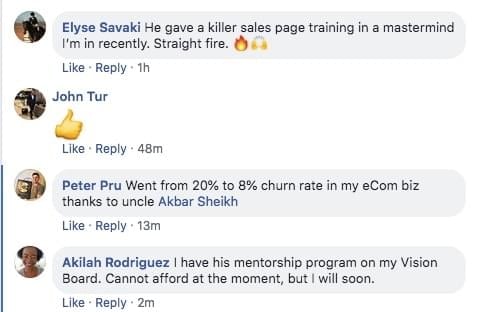
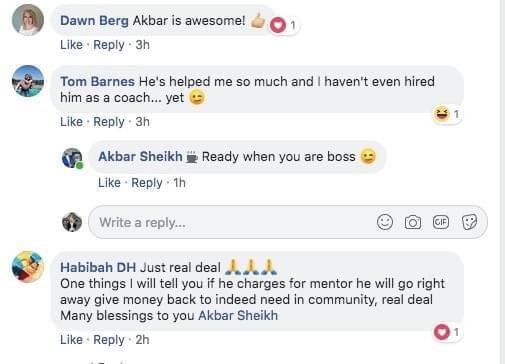
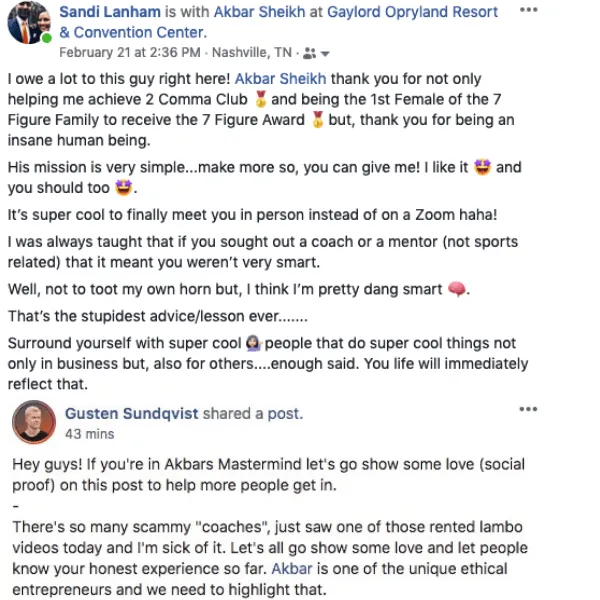
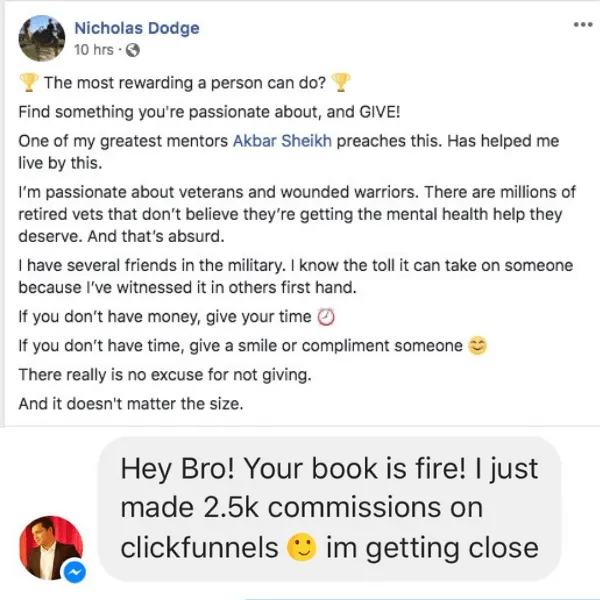
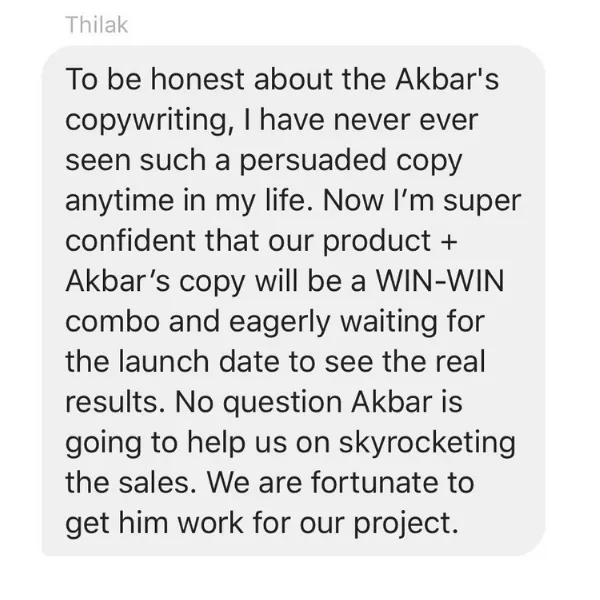
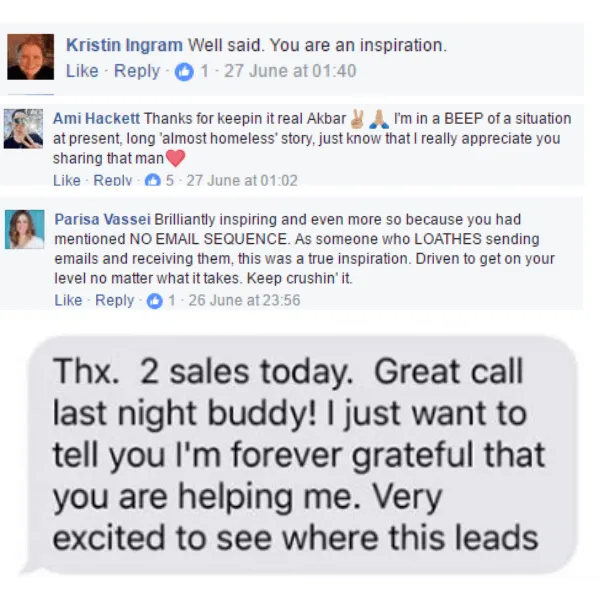

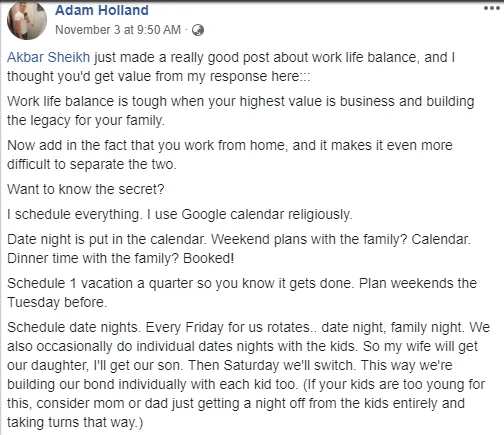
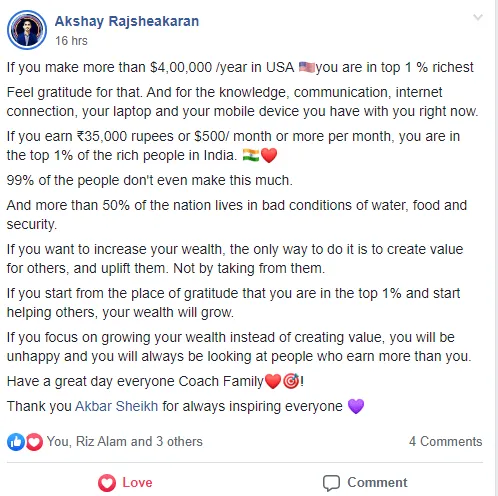
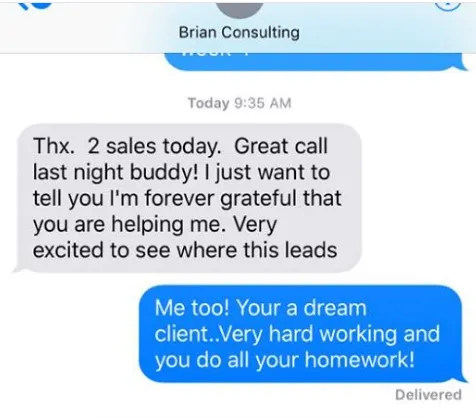

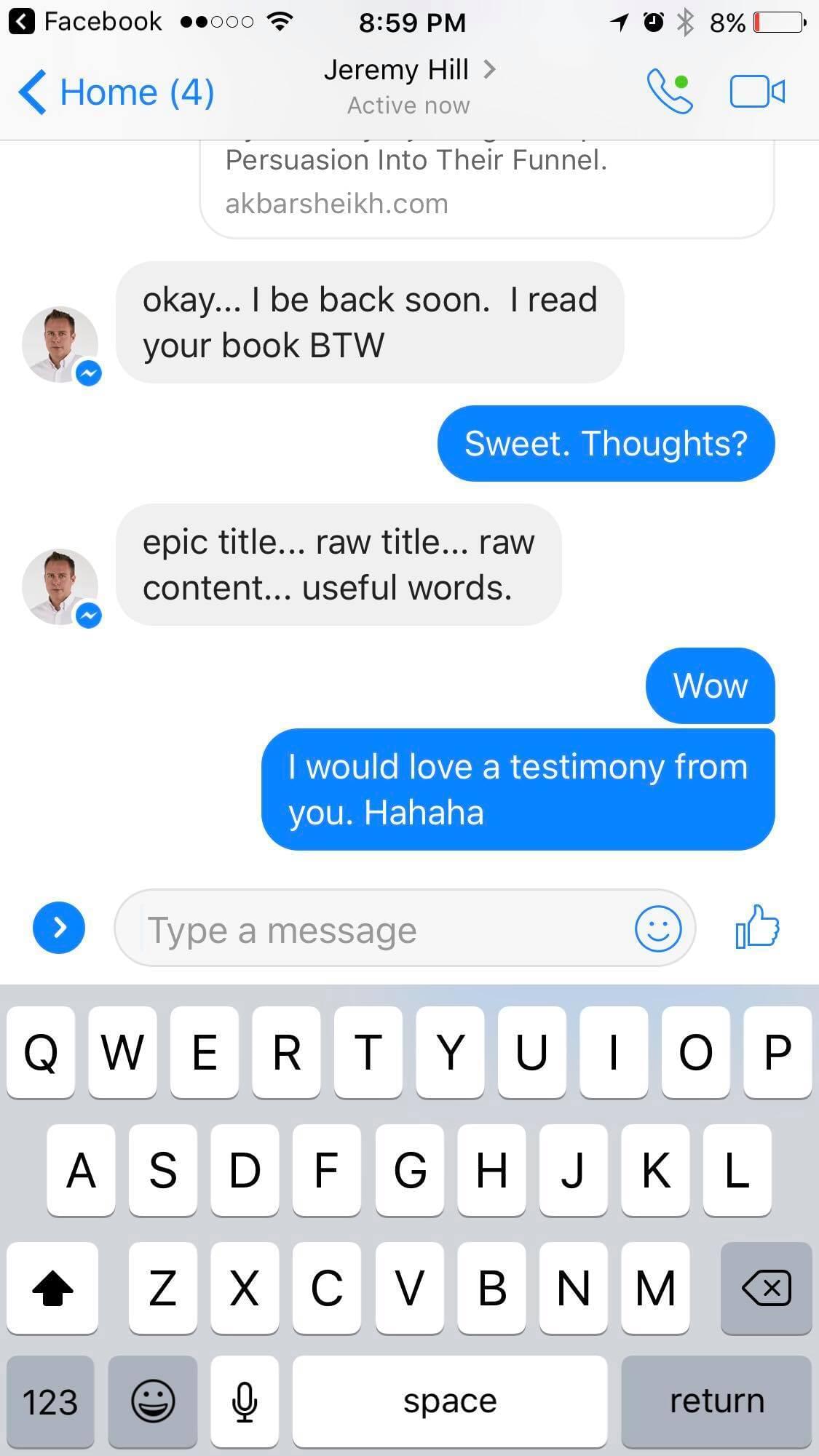


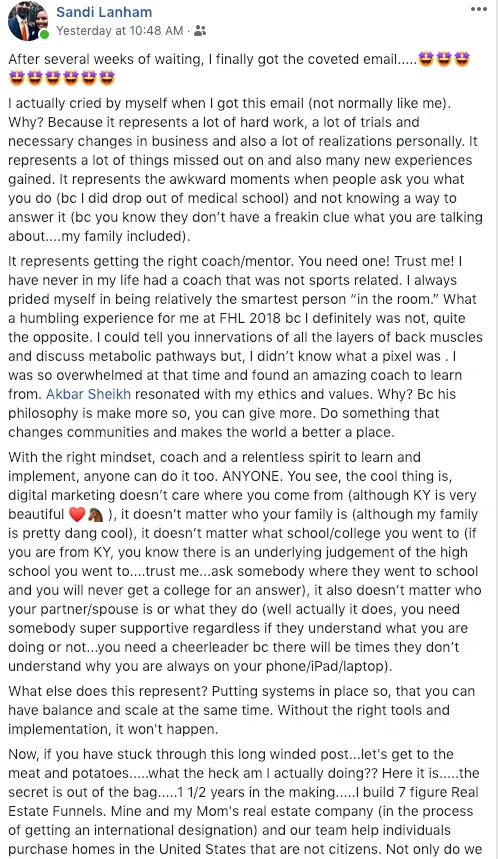
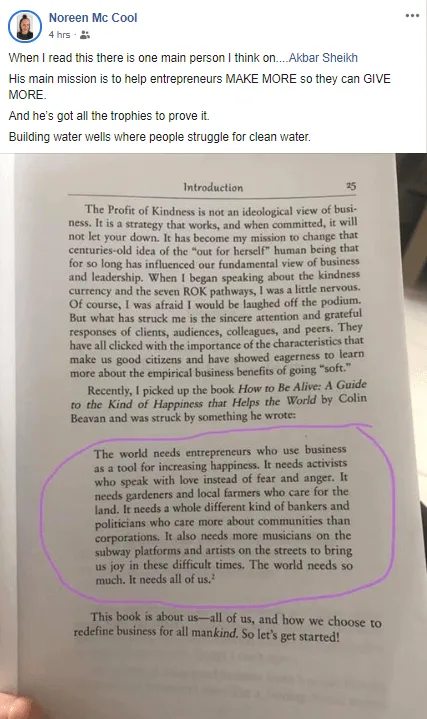

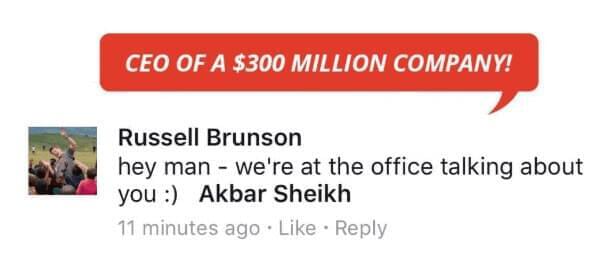
I could tell you all about our world-class coaching program, but let me show you instead...
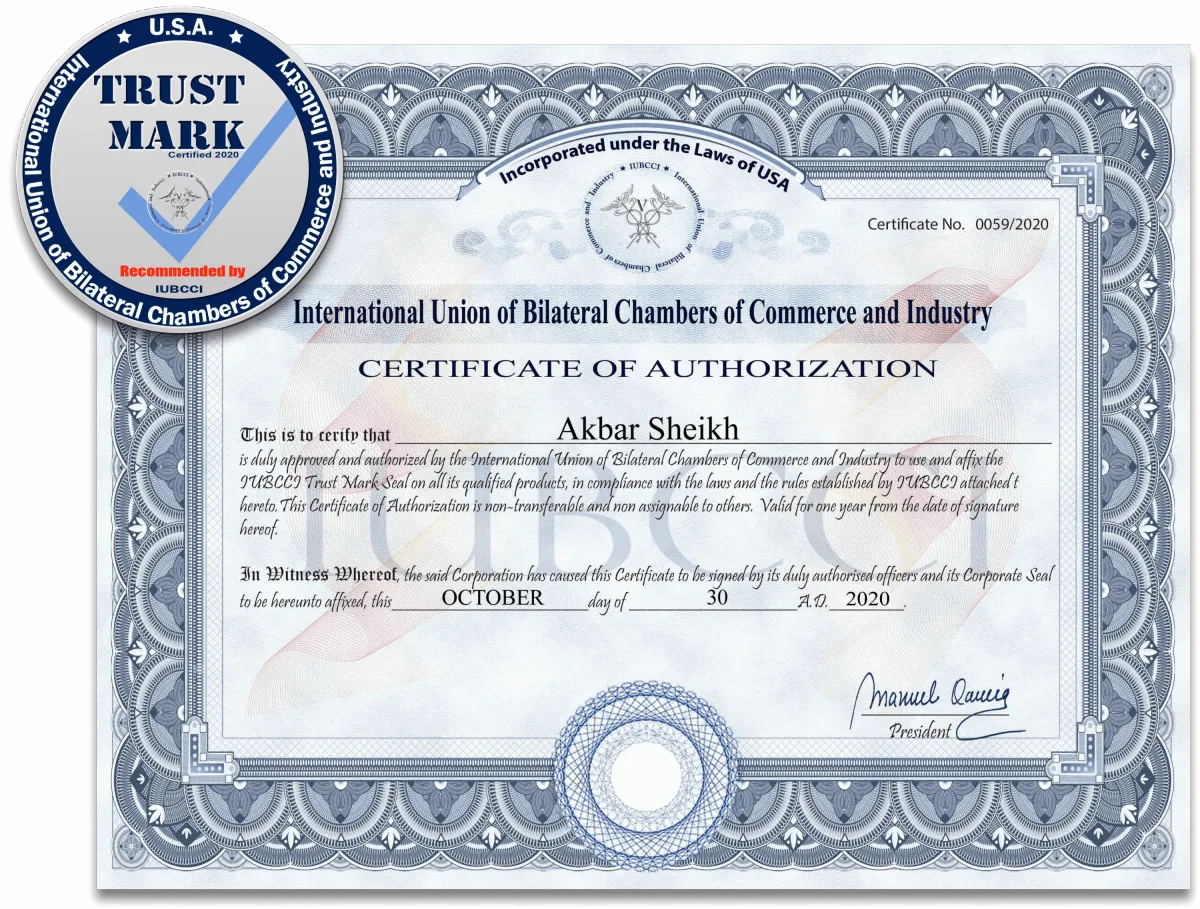
Award-winning coaching program
IUBCCI is one of the world’s largest business organizations, with an established presence in 50 countries, having 48 chambers of commerce members and over 20 international partnerships.
IUBCCI only awards the Trust Mark seal to organizations whose services or products meet high-quality standards. For a company to be awarded this distinction is an honor of the highest degree.
Frequently Asked Questions
FAQ 1
Answer 1
FAQ 2
Answer 2
FAQ 3
Answer 3
our industry leading guarantee
I personally guarantee that my dream team and I will work with you LIVE hands-on, every single day...
until you Get A Trophy!

The right fit?
THIS COULD BE RIGHT FOR YOU IF:
- You're an online entrepreneur or want to be one
- You have 1 hour a day to build your business
-
You’re ready to take imperfect action to scale
- You have the means to invest in your growth
-
You want to make more so you can give more
THIS MAY NOT BE RIGHT FOR YOU IF:
- You've never had any success online or offline
-
You’re looking to “get rich quick”
- You seek free advice without doing the work
- You don’t see the worth in self-investment
-
You want to make more and keep it all
So if that sounds good to you and you’re ready to leverage everything I’ve used to grow one of the most successful online businesses in our industry (including daily personal access to myself and my dream team), you know what to do...
Are you next?
Will you be next?...
Are you next?
Will you be next?...